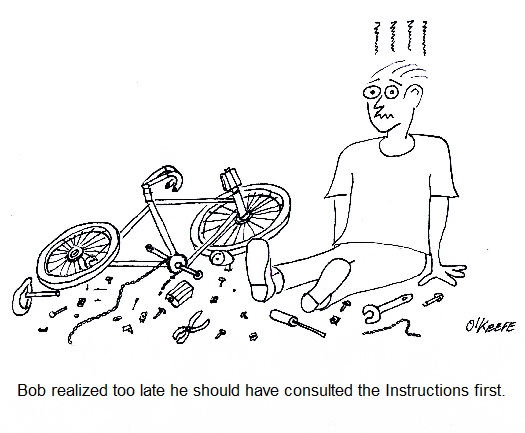
| You know those instructional inserts that come in just about everything you buy? If you’re lucky they’re a one-pager, showing a simple illustration of how your purchase works. But sometimes they’re multiple pages long, even approaching the length of a short story. This is often the case when the item in question is complex and contains many parts.
If you’re like some people you try to avoid reading these instructions, preferring to forge ahead to the assembly/usage stage as quickly as possible, and you’ve probably had your fair share of times that this approach didn’t pan out. You were forced to re-do things and crack open the instruction manual anyway. If the instructions were written clearly, you may have eventually come to regard them as indispensable. Clearly written instructions are one of the desired end results of the Development stage of the systems engineering approach to medical device design that we’ve been discussing. These instructions flow naturally from the finalized detailed design which has been produced earlier in this stage. Instructions aid consumers in the assembly, usage, and maintenance of the device, making for a satisfied customer. Instructions also aid in the efficient and proper manufacture of devices. Without them assembly personnel wouldn’t work as efficiently, and the end result might not be a desirable one. It’s easy for parts to end up where they don’t belong, adjustments to be off, etc. Just think about the last “assemble it yourself at home” project you were involved in. The desired result is for instructions produced to be well defined and capable of instructing line assembly personnel in the actual construction of the medical device that takes place during the Production stage. Subjects such as parts identification, assembly procedures, and layout of assembly lines are discussed, all of which are needed to plan out the manufacturing process effectively. The objective is to manufacture the devices in a cost effective manner and with minimum probability of defects. Next week we’ll continue our discussion on instructions, focusing on those that are produced during the Development stage that serve the purpose of guiding quality control technicians during the Production stage. ___________________________________________ |
Posts Tagged ‘medical device design’
Systems Engineering In Medical Device Design – Instructions, Part I
Monday, January 7th, 2013Systems Engineering In Medical Device Design – Concept Evaluation
Monday, December 17th, 2012| How many times have you bought something and lugged it home, only to discover that it didn’t work as advertised? These days this scenario is all too common. Chances are it was developed haphazardly and rushed into production without adequate research and testing. A chief contributor to the product’s not living up to expectations is very often the result of a poor beginning. In its concept and development stages, design engineers failed to use a systems engineering approach.
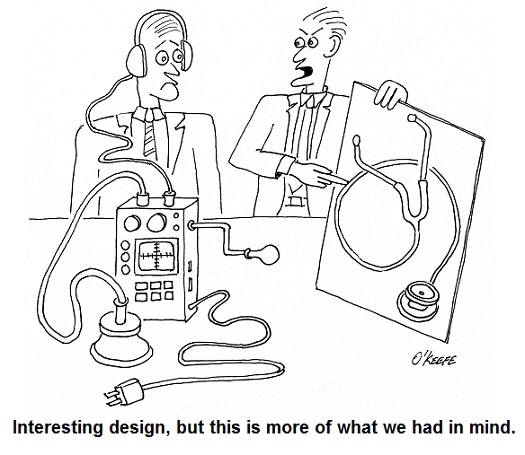
Last time our discussion of the Concept stage of systems engineering identified stakeholder requirements as being of three basic types, serving the needs of functionality, performance, and constraint. Once identified, these requirements were incorporated into a detailed specification that is approved by all stakeholders involved, then used to devise alternate medical device concepts in order to really size things up. Let’s now move on to the Development stage of the design process to see how the alternate concepts are evaluated. The Development stage of the systems engineering approach to medical design begins with research and development of alternate device concepts. Stakeholder requirements as defined in the original product specification are used to guide the process, then mockups and prototypes of the alternate concepts are built, tested, and analyzed in view of the requirements. Considerations such as cost, ease of manufacture, operation, durability, and potential risk of harm to users are evaluated. As often happens, the best alternate concept satisfies all but a few of the specified requirements, resulting in a “good enough” scenario. That is to say, if stakeholders can agree the requirements not met aren’t all that important in the scheme of things, they may be willing to remove them from the specification, thus approving the concept for further development. If an agreement such as this cannot be reached, it may be necessary to return to the Concept stage and begin the entire process again. This re-evaluation of the process should result in a set of requirements that are further refined and from which better options in alternative concepts can be developed. Next time we’ll continue our discussion of the Development stage and see what it takes to finalize design and begin manufacture. ____________________________________________ |
Systems Engineering In Medical Device Design – Concept and Requirements
Monday, December 10th, 2012| Last time we introduced the first phase of the systems engineering approach to medical device design, the Concept Phase. It’s a phase which emphasizes clear communication between design engineers and stakeholders in the project. Effective communication results in clearly defined stakeholder requirements.
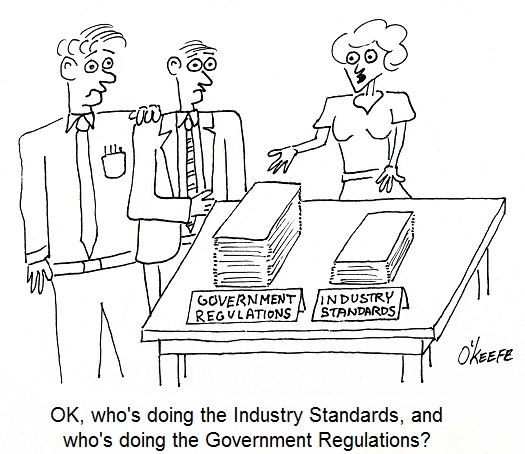
Stakeholder requirements are of three basic types, serving the needs of functionality, performance, and constraint. A functional requirement is a basic starting point, specifying the tasks to be accomplished by the system and its basic operation. For example, a medical diagnostic imaging device can be required to operate on a dedicated 15 amp branch circuit when plugged into a 115 volt wall outlet. Performance requirements delineate specific expectations as regards the system’s functionality, typically specifying parameters within which the system is to perform. For example, a medical device can be required to process a minimum number of test samples per hour. As for constraint requirements, they’re typically concerned with satisfactorily complying with both governmental regulations and industry standards. Governmental regulations include those established by the US Food and Drug Administration, as well as any applicable foreign agencies that may be involved should the medical device be introduced to other countries. Once the draft specification is written, design engineers review it in painstaking detail. Stakeholders’ requirements must all be accounted for and interpreted correctly. This is typically done by sitting down with each stakeholder and reviewing the draft. Finally, each stakeholder’s signature is obtained, signifying their approval. Now complete, the approved specification is used as a roadmap to guide project development through to the next and final step of the concept stage, devising alternate medical device concepts. Why discuss alternate concepts? Just like consumer comparison shopping for TVs and other goods, you’ve got to have a basis of comparison in order to make a sound judgment. This holds true for the medical device industry as well as private households. Next time we’ll proceed to the next stage of the design process, Development. We’ll see how alternate concepts are evaluated to find the best overall option, thus beginning the actual design process leading to manufacture. ____________________________________________ |
Systems Engineering In Medical Device Design – Concept and Communication
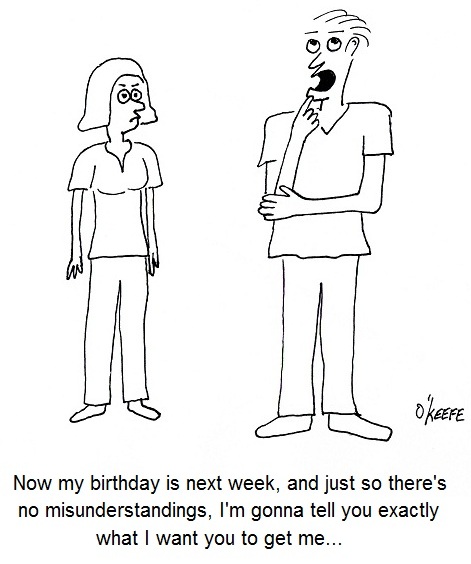
Monday, December 3rd, 2012| “Ask and you shall receive,” like “Make your thoughts known,” have the same objective, to initiate a dialogue between someone with a vision and those who can get the job done. In other words, if you don’t ask for it, you’re probably not going to get it, and the moving force behind it all is communication. Communication is as important in design engineering as it is in marriage.
Last time we learned that a system is a combination of interacting components organized to achieve one or more specific purposes and that communication is a key ingredient in the process. Now let’s see how the systems engineering approach is used within the medical device design process. The systems engineering approach consists of five key stages, the first being Concept. In this stage the objective is to identify all stakeholders, that is, those who have a stake in the outcome, then exhaustively define and capture their requirements. Crucial to this stage is a good line of communication between design engineers and stakeholders. This usually takes the form of brainstorming sessions in which all parties meet to toss around ideas. These ideas eventually solidify into design requirements. Once the design requirements are identified, they are incorporated into the first draft of a working specification. This specification will be written using plain English to minimize any potential misunderstandings. Within the specification each requirement is not only well defined, but traceable back to whoever proposed it. To this end, all requirements are listed in tandem with the names of stakeholders proposing them. Accountability is the main concern here. Next time we’ll talk more about these design requirements, and how they must serve the needs of functionality, performance, and constraint. ____________________________________________ |
Systems Engineering In Medical Device Design – Introduction
Monday, November 26th, 2012Medical Device Design Controls – Planning and Input
Sunday, August 29th, 2010| Have you ever had the divine experience of remodeling a major-use room of your house? Was the general contractor you employed able to understand what you wanted, plan out the work according to your requirements, and finish the job to your satisfaction? Maybe you had the unfortunate experience of hiring one that forgot your requirements, made things up as they went along, and stuck you with a room that looked awful, violated building codes, and didn’t meet your needs.
Now imagine what would happen if a medical device company took this haphazard approach to designing new products. Suppose the company’s engineers ignored the input of regulatory, marketing, procurement, quality control, and manufacturing staff? What if they chose not to follow applicable industry standards for performance and safety? And what if they failed to check design calculations or test prototypes for errors before putting the device into production and introducing it to the marketplace? The result is likely to be unfavorable, just like your contractor forgetting that you wanted a black granite countertop, not a beige one. To help eliminate painful and costly scenarios such as these, the FDA requires that medical device manufacturers establish and maintain procedures to control the design of Class II and III devices, and even some Class I. This requirement for a system of design controls is part of the Quality System Regulation (QSR) under Title 21 of the Code of Federal Regulations. In case you’re not too familiar with the Code of Federal Regulations, Title 21 gives the FDA legal authority to regulate food, drugs, and medical devices in the United States. So what falls under the premises of FDA design controls? Well, the FDA requires that a medical device company develop procedures for:
For now, let’s focus on Design and Development Planning and Design Input Procedures. In the Design and Development Planning Procedure companies must carefully plan who will be involved in each phase of product development, as well as how they will interact, all in an effort to ensure that information flows and design requirements are met. The right pool of people would include design engineers, in addition to those employees responsible for making sure that regulations are complied with and those who are charged with securing intellectual property rights to the design. Then there are those who must acquire the physical materials required to manufacture the device and those who will do the actual manufacturing of it. Also, those responsible for quality control, marketing, sales, and product service should be involved. Perhaps others should be involved as well. Mind you, the Design and Development Planning Procedures are not set in stone. They must be regularly reviewed and updated as the project evolves. Now let’s talk about Design Input, which is another term for a design requirement. These inputs can come from inside or outside the company. An example of a requirement coming from within is when Marketing stipulates that the maximum manufacturing cost of the device should not exceed $150 in order to maintain an acceptable margin of profit and be most competitive in the marketplace. A design requirement coming from outside the company would include industry standards that make specific requirements, such as requiring that the device in question be designed to protect its electronics from radio frequency interference. Next time we’ll continue our discussion on medical device design by exploring Design Output, Design Verification, and Design Review Procedures. _____________________________________________ |
FDA Classifications for Medical Devices – Special Controls
Monday, August 23rd, 2010|
For the last couple of weeks we’ve been discussing FDA medical device risk classifications, namely Classes I, II, and III. We also began discussing the FDA system of regulatory controls governing each class, starting with General Controls. This week we’ll examine the more stringent guidelines that come into play within Special Controls. As you would imagine from the name, Special Controls come into play when General Controls aren’t deemed to be sufficient to deal with the situation. Class II and III medical devices, because they pose a higher level of risk to patients than Class I, generally require more FDA supervision than mere General Controls. These devices tend to fall under the auspices of Special Controls. Special Controls include things like special labeling requirements, complying with mandatory performance standards, and perhaps requiring that a manufacturer conduct a Post Market Surveillance (PMS) study. In case you’re wondering, a PMS may be required by the FDA to collect data after a medical device is sold, should there be any unexpected adverse events involving the device. A study of this data would aid in an investigation to determine the number of events, the cause of the events, and how to correct any problems that led to the events. Let’s look at some examples of how Special Controls apply to Class II medical devices. One example would be a cranial molding helmet. These helmets are often used with infants to reshape their skulls into becoming more symmetric. Due to the nature of this device’s application on such a delicate patient, Special Controls include a requirement for special labeling. In this case, the labeling must include warnings to physicians and parents that precautions must be taken during its application to protect patients from possible injury, including eye trauma and impairments of brain growth. Another example would be sutures. Yes, they are considered to be Class II medical devices. In this case, Special Controls require that sutures meet “mandatory performance standards.” What are “mandatory performance standards?” Well, they generally include industry consensus standards for particular medical devices. They are based on industry-wide accepted guidelines to ensure proper product performance. In this example, industry standards for suture material contain specific guidelines as to material composition, diameter size, mechanical strength, and biocompatibility. Adherence to these standards provides the highest assurance that sewn incisions won’t break open when the suture is stressed or the suture material won’t cause some sort of adverse reaction with the patient’s skin. As specific as Special Controls can be, they are sometimes not enough. On these occasions the FDA states, “Class III devices are those for which insufficient information exists to assure safety and effectiveness solely through General or Special Controls.” Under these circumstances more regulatory control may be imposed. This is the case when dealing with medical devices directly responsible for supporting/sustaining human life, such as a cardiac defibrillator. One such FDA control method that goes beyond Special Controls is the requirement to submit a Pre Market Approval application (PMA) to the FDA for approval. This PMA is subject to the most stringent FDA requirements. As a part of the PMA process a company must demonstrate the safety and effectiveness of a new medical device design by producing data and documentation obtained during “adequate and well-controlled” clinical trials. In our series on FDA Classifications for Medical Devices we have merely grazed the surface. Depending on the device in question there may be a myriad of other considerations, so please consult the FDA’s web site for the complete picture: http://www.fda.gov/MedicalDevices/default.htm. _____________________________________________ |
FDA Classifications for Medical Devices
Sunday, August 8th, 2010|
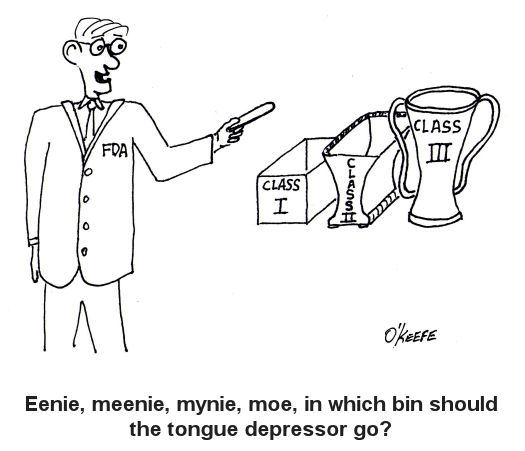
Hardly a week goes by that the FDA, that is the Food and Drug Administration, is not in the news. From the recall of drugs found to be harmful after the fact, to investigations of medical device suppliers and inspections of salmonella contamination at meat processing plants, the FDA is responsible for overseeing and regulating a wide range of products and processes. It’s stated purpose being: The FDA is responsible for protecting the public health by assuring the safety, efficacy, and security of human and veterinary drugs, biological products, medical devices, our nation’s food supply, cosmetics, and products that emit radiation. http://www.fda.gov/AboutFDA/WhatWeDo/default.htm From its humble beginnings at the beginning of the last century as the Pure Food and Drug Act, it has grown to regulate more than $1 trillion worth of consumer goods, about 25% of that said to be attributable to consumer goods expenditures in the United States. In 1976, the FDA began classifying medical devices, using a three-tiered system to distinguish them according to level of risk to patients. Class I devices present the lowest level of risk and requires the least regulatory control, while Classes II and III represent higher levels of risk. Just to give you some perspective, Class I medical devices include things like tongue depressors, bedpans, arm slings, and hand-held surgical instruments. In the Class II category are things like surgical drapes, blood pressure cuffs, catheters, wheelchairs, heating pads, and x-ray film processing machines. And I’m sure you’ve guessed by now that Class III devices are for the heavy-hitters, including things like defibrillators, heart valves, and implanted cerebral stimulators. So why does the FDA classify medical devices? Practicality is one key reason. It would be highly impractical, if not downright impossible, for the FDA to subject manufacturers of low risk Class I devices, like tongue depressors, to the same scrutiny as manufacturers of Class III devices, such as heart valves, etc. Along with miles of red tape would come a huge financial burden that would effectively raise the price of your common tongue depressor through the roof and, undoubtedly, force the manufacturer out of business. Hand in hand with medical device classifications are regulatory controls imposed by the FDA. We’ll see how they fit into the picture next time. _____________________________________________ |